2014, Vol 12, No 2
Zasady stosowania dootrzewnowej chemioterapii w hipertermii (HIPEC) w leczeniu nowotworów złośliwych powierzchni otrzewnej w połączeniu z zabiegami cytoredukcyjnymi: zalecenia krajowe
Piotr Rutkowski, Beata Śpiewankiewicz, Krzysztof Herman, Tomasz Jastrzębski, Józef Kładny, Zbigniew Kojs, Maciej Krzakowski, Wojciech Polkowski, Lucjan Wyrwicz, Piotr Wysocki, Marcin Zdzienicki, Wojciech Zegarski
CURR. GYNECOL. ONCOL. 2014, 12 (2), p. 86–97
DOI: 10.15557/CGO.2014.0009
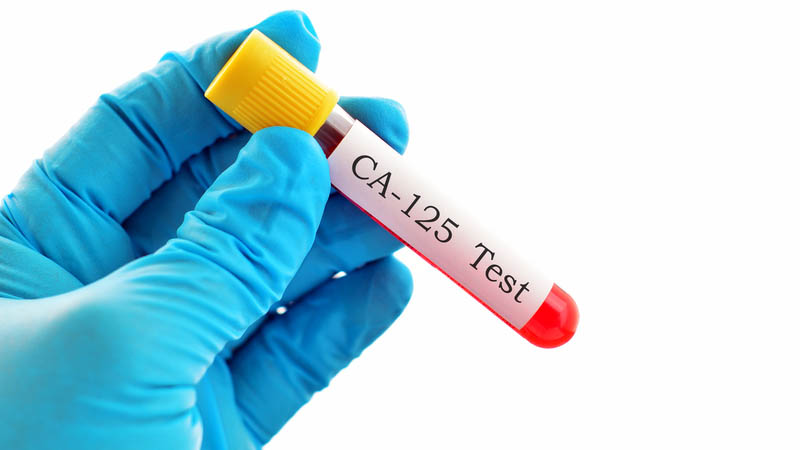
Znaczenie obserwacji pacjentów z nowotworem ginekologicznym: doświadczenie jednego ośrodka na Słowacji
Erik Lajtman, Miloš Mlynček, Mária Zajacová
CURR. GYNECOL. ONCOL. 2014, 12 (2), p. 98–114
DOI: 10.15557/CGO.2014.0010
Wpływ wybranych indywidualnych czynników klinicznych na odtwarzalność obszaru napromieniania u chorych leczonych z powodu nowotworów ginekologicznych
Bogusław Lindner, Ryszard Krynicki, Marta Olszyna-Serementa, Agnieszka Nalewczyńska, Anna Zawadzka, Katarzyna Bednarczyk, Piotr Czuchraniuk
CURR. GYNECOL. ONCOL. 2014, 12 (2), p. 115–124
DOI: 10.15557/CGO.2014.0011
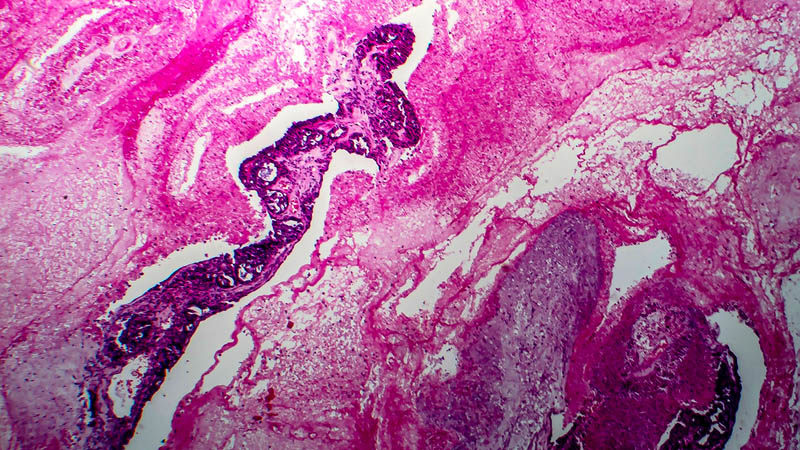
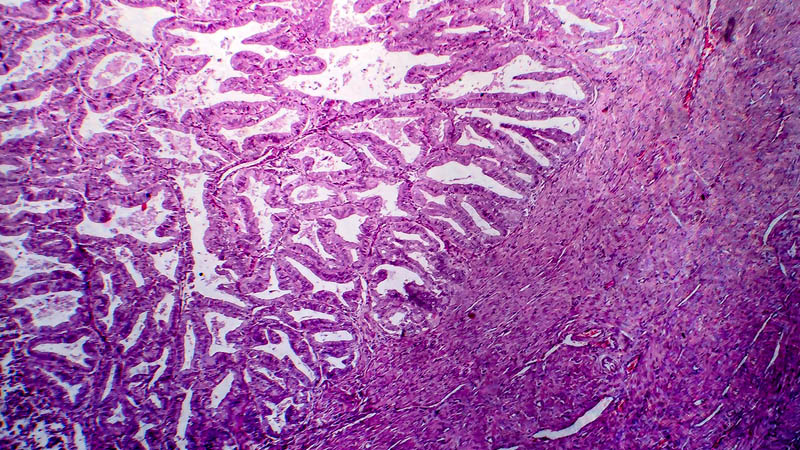
Ograniczenia w leczeniu chirurgicznym raka jajnika
Michał Makarewicz, Krzysztof Koper, Beata Śpiewankiewicz, Andrzej Budzyński, Tomasz Rajs, Zbigniew Kojs, Tomasz Bieda, Łukasz Wicherek
CURR. GYNECOL. ONCOL. 2014, 12 (2), p. 140–154
DOI: 10.15557/CGO.2014.0013
Leczenie chirurgiczne zaawansowanego raka szyjki macicy a wytrzewienie – przegląd literatury
Paweł Mach, Kinga Krokowska, Andrzej Stelmach, Jerzy Siekiera, Maria Szymankiewicz, Beata Śpiewankiewicz, Zbigniew Kojs, Krzysztof Koper, Łukasz Wicherek
CURR. GYNECOL. ONCOL. 2014, 12 (2), p. 125–139
DOI: 10.15557/CGO.2014.0012
Komunikacja z rodziną pacjenta chorego onkologicznie
Bożena Winch
CURR. GYNECOL. ONCOL. 2014, 12 (2), p. 155–171
DOI: 10.15557/CGO.2014.0014
Czy badanie ginekologiczne zapewnia prawidłowe ustalenie stopnia klinicznego zaawansowania w raku szyjki macicy bez badań obrazowych? Na podstawie opisu przypadku
Ryszard Krynicki, Agnieszka Nalewczyńska, Bogusław Lindner, Jakub Pałucki, Beata Śpiewankiewicz
CURR. GYNECOL. ONCOL. 2014, 12 (2), p. 172–178
DOI: 10.15557/CGO.2014.0015