2012, Vol 10, No 4
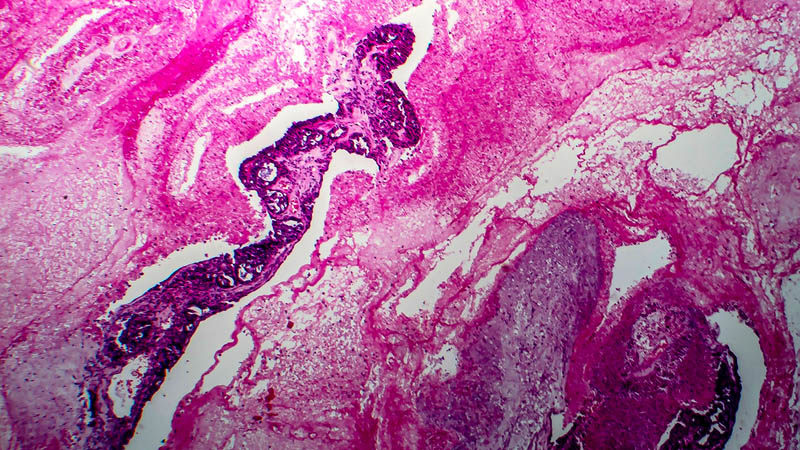
Analiza porównawcza immunoreaktywności metalotioneiny w zaśniadzie groniastym i w doczesnej w zależności od zastosowanego leczenia – wyłącznie operacyjnego albo operacyjnego z uzupełniająca chemioterapia
Paweł Basta, Magdalena Dutsch-Wicherek, Marta Biedka, Krzysztof Koper, Paweł Mach, Krystyna Gałązka, Tomasz Basta, Michał Leśniak, Beata Śpiewankiewicz, Łukasz Wicherek
CURR. GYNECOL. ONCOL. 2012, 10 (4), p. 261-269
DOI:
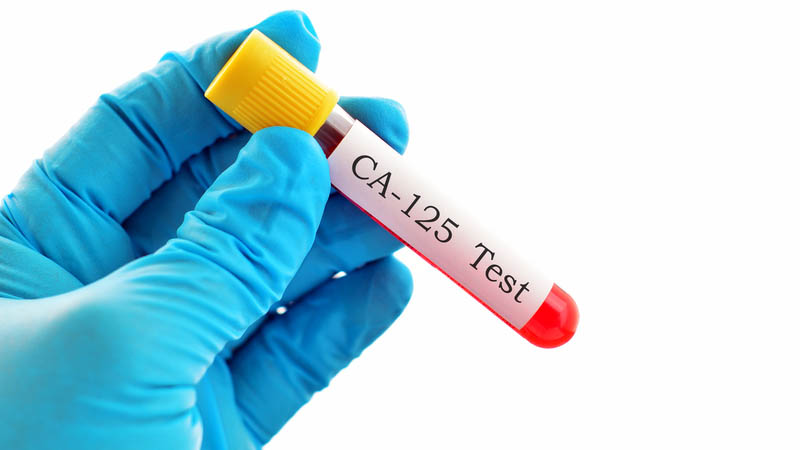
Nowotwory złośliwe i stany przedrakowe narządu płciowego stwierdzane u pacjentek nosicielek mutacji konstytucyjnych genu BRCA1 poddanych operacjom profilaktycznym usunięcia przydatków
Janusz Menkiszak, Anita Chudecka-Głaz, Ryszard Bedner, Jacek Gronwald, Małgorzata Wężowska, Zbigniew Kojs, Izabella Rzepka-Górska
CURR. GYNECOL. ONCOL. 2012, 10 (4), p. 270-285
DOI:
Zastosowanie śródoperacyjnej radioterapii u chorych na wczesnego raka piersi – ocena efektywności i toksyczności leczenia
Bartosz Urbański, Andrzej Roszak, Krystyna Bratos, Żaneta Wareńczak-Florczak, Hanna Włodarczyk, Piotr Milecki, Aldona Karczewska-Dzionk, Dawid Murawa, Ewa Wierzchosławska
CURR. GYNECOL. ONCOL. 2012, 10 (4), p. 286-295
DOI:
Analiza wybranych problemów biopsji węzła wartownika u chorych z rakiem piersi
Tomasz Nowikiewicz, Marta Biedka, Edward Krajewski, Krzysztof Koper, Wiesława Windorbska
CURR. GYNECOL. ONCOL. 2012, 10 (4), p. 296-306
DOI:
Podstawy immunologiczne powstawania i leczenia nowotworów kobiecego układu płciowego
Michał Leśniak, Magdalena Dutsch-Wicherek, Krzysztof Koper, Tomasz Basta, Michał Makarewicz, Beata Śpiewankiewicz, Łukasz Wicherek
CURR. GYNECOL. ONCOL. 2012, 10 (4), p. 307-316
DOI:
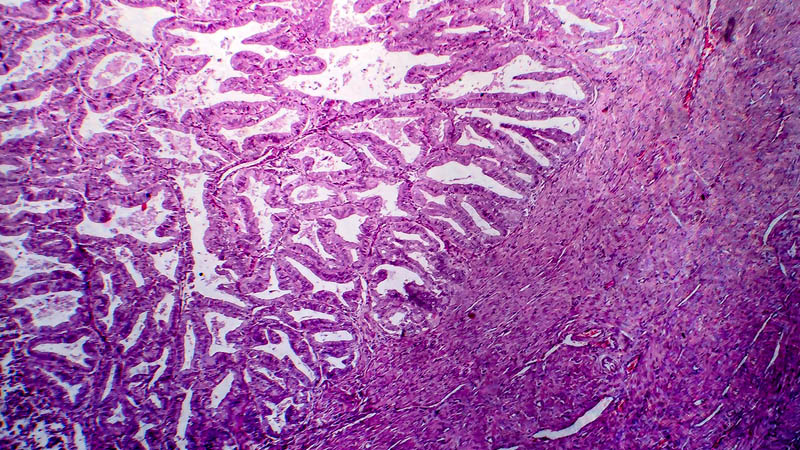
Rak jajnika – czy zawsze chirurgia?
Rafał Moszyński, Stefan Sajdak
CURR. GYNECOL. ONCOL. 2012, 10 (4), p. 317-325
DOI:
Szczególne postacie kliniczne nowotworów złośliwych piersi
Janusz H. Piekarski
CURR. GYNECOL. ONCOL. 2012, 10 (4), p. 326-336
DOI: